This content is being reviewed in light of recent changes to federal guidance.
Henrietta Lacks: The Immortal

PC: Bridgeman Images
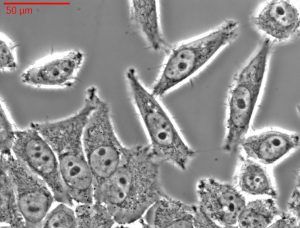
If you ever took a class on medicine or human biology, you may have heard of the HeLa cell line. You may have learned that they were the first human cells to be successfully cloned, that HeLa is the oldest and most researched cell line in history, or that HeLa cells have been used to test the polio vaccine, used in cancer research, and even sent into space. You may not have learned how the HeLa cell line came to be and the important discussion it brought to light regarding informed patient consent.

It all started when Loretta Pleasant, later Henrietta Lacks, was born on August 1, 1920, in Roanoke, Virginia. The name Henrietta came from the nickname Hennie that her family gave her growing up. Her mother died during childbirth when Lacks was just four years old. Her father, unable to care for all ten children on his own moved the family to the small town of Clover, Virginia, where the children were split among extended family members. Lacks ended up with her maternal grandfather.
On January 29, 1951, Lacks went to Johns Hopkins in Baltimore Maryland, the only hospital in the area that treated Black patients, because she was experiencing pain in her abdomen as well as some bleeding. She had hesitated because of the treatment Black patients typically received at the time. Lacks described a “knot” in her stomach, which the doctor ignored, telling her only that she was pregnant. It wasn’t until after she gave birth and had severe hemorrhaging that her doctors did a biopsy. The misdiagnosis at the time was a malignant epidermoid carcinoma¹ of the cervix. In 1970 research revealed that she actually had adenocarcinoma².
PC: Biomol
During her treatment, two samples were taken from her cervix without her knowledge or consent. One set of the samples taken were healthy and the other, cancerous. The cells collected from Lacks were given to Dr. Otto Gey, who had been unsuccessful up to that point in keeping cells alive. Henrietta’s cells were the first to survive and reproduce after being separated from the body. The cancerous cells would become some of the most researched cells in history and are part of the immortal HeLa cell line. Lack’s cells continue to been used in medical research globally.
PC: Sutori
Research on the HeLa cell line has furthered the advancement of medicine in many fields. Their ability to reproduce rapidly, they have been used in vaccine research, cancer research, and even COVID-19 research. Henrietta’s cells have helped develop drugs for treating herpes, leukemia, influenza, hemophilia, and Parkinson’s disease. They have been used to study lactose digestion, sexually transmitted diseases, appendicitis, and human longevity. The use of these cells is infinite, and their lifetime is eternal.
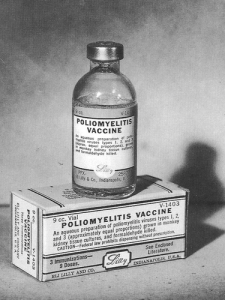
One of the first major uses for the HeLa cells was the development of the polio vaccine. The research done on the cells using the virus that causes polio helped create the vaccine that every child now gets. The ongoing impact of the HeLa cells use can be seen in radiation for cancerous cells and AIDs research. The use of HeLa cells in COVID-19 research has allowed for a greater understanding of the mechanics of the SARS-COV-19 virus, which can be used to curate treatment of the disease.

However, the successful story of advances in health and medicine is not all good. These cells were taken without the consent of Henrietta Lacks or anyone in her family. The family only learned that her cells were taken when there was a mix-up in a lab. Twenty years after Henrietta’s death, the family was contacted about providing samples to help differentiate between Henrietta’s cells and the cells of other people. The cells were taken at a time when a patient’s consent was not required. As a result, the practice of cell harvesting without consent was very common. Because the cells were used for public experimentation, her records became public in 1980, again, without the consent of her family.
Although Henrietta Lacks made amazing contributions to science and medical research her story is a great example on why informed consent is crucial. Not only was this a lack of consent, but there was also no knowledge provided about the use of her cells. As a result, the family received neither the credit nor the compensation they deserved.
There is a long and dark history of medical experimentation on Black people by medical professionals who take advantage of an inequitable system compounded by racist practices historically especially with regard to the African American community. While Henrietta’s cells have led to major gains in the field of medicine, her family still lives with limited access to healthcare, unable to access the very medicines Henrietta made possible. Henrietta’s story is significant because of the ongoing meaning of her life to science and medicine. At the same time, that she was never made aware of the way in which her body was being used or was unable have a say in it is a travesty. Even with safeguards against the this type of exploitation, we still have a long way to go in addressing the systemic nature of racism as it operates in health care and medical research.
 More on Henrietta Lacks
More on Henrietta Lacks
Rebecca Skloot’s book The Immortal Life of Henrietta Lacks.
https://www.nature.com/articles/d41586-020-02494-z
https://www.hopkinsmedicine.org/henriettalacks/
https://www.npr.org/2010/02/02/123232331/henrietta-lacks-a-donors-immortal-legacy
¹epidermoid carcinoma: Epidermal (skin) cancer which forms from squamous cells and usually appear in hollow organs such as the digestive system and respiratory track.
²adenocarcinoma: A type of cancer that begins in mucus producing glandular cells.
 Aubrey Kerbs is an undergrad student majoring in history. After graduating next spring with a history BA, Aubrey will be pursuing a master’s in Library and Information Sciences. Afterwards Aubrey will be looking for work at either university libraries or government libraries. The goal is to one day work at the Smithsonian Institute. Aubrey works as a research assistant with the BBIP team.
Aubrey Kerbs is an undergrad student majoring in history. After graduating next spring with a history BA, Aubrey will be pursuing a master’s in Library and Information Sciences. Afterwards Aubrey will be looking for work at either university libraries or government libraries. The goal is to one day work at the Smithsonian Institute. Aubrey works as a research assistant with the BBIP team.